Battling With...Standard Treatments (Western)
Standard Western Treatments
Over the years that I’ve been battling the grade 4 GBM, not much has changed in the standard treatments. Starting with surgery (if operable), then radiation, and then chemotherapy. Since I was diagnosed 16 years ago, only Temodar, Avastin and Optune have been FDA approved. Some patients are hesitant to go through surgery, radiation, or chemo when they are diagnosed. Statistics show it does not really add much survivorship. And it’s overwhelming to think of a doctor invading your brain with surgery, or seriously covering parts of your brain with radiation, or taking a chemo that kills off brain cells. However, I personally believe that it’s the needed line of treatments to start with. I don’t think I would be here, 16 years later if I had not been through the six brain surgeries, the two radiation treatments, and on Temodar chemo over 3 years. And I never regret taking them all. I’ll try to share some of what I learned while I went through the three standard treatments; surgery, radiation and chemotherapy. See below for the summary of my 16 years through the standard treatments…

June 2000 – Dx Grade 4 Glioblastoma Multiforme
I was 33 years old. I started having a really bad headache in my left temple. An MRI showed a pocket of blood clustering in my brains left temporal lobe. I had brain surgery at OHSU in Portland Oregon. The neurosurgeon removed an acorn sized Grade 4 GBM surrounded by an Arterial Venial Malformation (AVM) in my left temporal lobe.
Then I went into a radiation clinical trial at UCSF in San Francisco Ca. called H-boc, where they injected me with cow hemoglobin and gave me high oxygen right before the radiation hypothetically to reduce hypoxia and increase the radiation ability. Two weeks in to the clinical trial I had an allergic reaction to the H-boc – so had to finish the regular conformal radiation at home in Medford, Or. After the surgery and radiation, I began getting an MRI every 2-3 months
August 2004 – 1st GBM recurrence. “Awake” brain surgery at UCSF with Dr. Berger, removed the grape sized GBM from the edge of the tumor cavity in my left temporal lobe. Did the awake surgery to reduce the risk of losing language? Karnofsky Score 90. After surgery I took 330mg Temodar chemotherapy on the 5/23 schedule for 1/5 years. MRIs every two months at UCSF and saw the neuron-oncologist Dr. Butowski.
February 2007 – 2nd GBM recurrence. Had the WADA test before surgery to see if I was left or right brain dominated. I am left handed, and there was a small chance I was right brain dominated. If so, my whole left temporal lobe could have been completely removed without taking away my language. But the test resulted showed that I was left brain dominated like most people. So I went into “Awake” brain surgery at UCSF with Dr. Berger again, and he fully removed the pea sized GBM and a “buffer” around it the size of a golf ball trying to get any hidden cancer cells. Again, the tumor was located on the edge of the tumor cavity in my left temporal lobe. Karnofsky Score 90. Back on Temodar 330mg on the 5/23 schedule for 2 years. MRIs every two months at UCSF and seeing my neuron-oncologist Dr. Butowski.
March 2009 – 3rd GBM recurrence Brain surgery at UCSF with Dr. Berger to remove the approx. 4mm tumor in the meninges located over the tumor cavity. All seen tumor was removed. Pathology confirmed it was the GBM back. The genetic test came back that my GBM was not the type to respond well to Temodar. Dr. Butowski recommended that we “keep an eye on it”, with MRIs every two months. No treatments.
March 2013 – 4th GBM recurrence Went through my 5th brain surgery at UCSF with Dr. McDermott. The small tumor was again located in my meninges on the surface of my left temporal lobe area. All seen tumor was removed. Since my genetic tests came back negative for EGFR and negative for the deletion of the PTEN, I decided to not take any western med treatments and only take the natural alternative treatments to boost my own immune system (many supplements, eating healthy and organic, exercise, simplifying life, and leaning on God for strength.) I get MRIs every 2 months.
After this 2013 surgery my neuro-oncologist Dr. Butowski at UCSF had some tumor tissue sent off for these genetic tests. The results were GFAP – neoplastic cells are strongly positive, OLIG2 – majority of cells strongly positive, P53 – positive in a subset of tumor cells (approx. 15% focally), NFP – primarily positive at the periphery, with a few entrapped axons present, IDH1 – neoplasm is negative, EGFR – negative for EGFR amplification, PTEN – negative for PTEN deletion.
May 2014 – 5th GBM recurrence Went through my 6th brain surgery at UCSF with Dr. Berger. Two small tumors were removed, 4mm and 7mm, located on the edge on my existing tumor cavity. Genetic tests showed that only 30% of the tumor was GBM and 70% “gliosis” which I was told was like alive growing scar tissue. This was pretty good news, maybe the DCA, metformin and medical marijuana I am taking helped! So I am continuing to take those three things and the many supplements and other things I do. At this point I am not on any chemotherapy or any other “western med” treatments. I keep getting MRIs every two months, and so far they have looked clear, no seen tumor.
August 2015 – 6th GBM recurrence This was my first recurrence that was considered inoperable. The tumor was located adjacent to a critical artery and was too risky to remove; according to Dr. Berger at UCSF (and I trust him!). So I had the Gamma Knife Radiation. I was hesitant at first and nervous, but it ended up being a one day “easy” treatment! I had it with Dr McDermott at UCSF. The MRI showed that within 2 months after the Gamma Knife 1/2 of the tumor disappeared. Then within 4 months the MRI looked beautifully clear, no seen tumor at all!
March 2017 – Biopsy & diagnosed with aPXA in the pituitary. In April I went through 5 weeks of radiation.
November 2018 – Reoccurrence of GBM, located in my left temporal lobe again. Because of the small size of this reoccurrence, I will be going through Gamma Knife radiation.
There is one point I must start with. It actually applies to all of the standard treatments. It’s that you must find an excellent brain neuro….. surgeon, oncologist and radiologist. Many, actually most, of the hospitals in the USA do not specialize in brain tumors. They may have a neurosurgeon, but more not often a doctor that specializes in “brain” neurosurgeon.
Neurosurgeons at a more “general” hospital maybe only do four brain surgeries in a year; where a neurosurgeon in a hospital that specializes in brain tumors mostly likely does up to four brain surgeries a day. That makes a big difference, and statistics show that patients treated in hospitals that do not specialize in it; do not live as long.
So if you want to beat statistics and become a long term survivor, it’s best to find a GREAT brain tumor hospital. They are limited. I live in a small town in Oregon that does not have one; actually the whole state of Oregon does not have one. Consequently, I decided to make to the long 7 hour drive south to be at one of the best brain tumor hospitals on the west coast, UCSF in San Francisco, Ca. It’s well worth the drive.
My GBM tumors have always appeared in my left temporal lobe, that plays a key role in language and memory, which I had a high risk of losing. I’m sure the “neurosurgeon” here in the little town of Klamath Falls, Oregon would have told me it was inoperable. Just because of their lack of experience.
At UCSF, Dr. Berger has done what I consider art work in my brain! I’ve always come out of surgery beautifully; able to talk, remember who I was, and much more. Two of my surgeries were even done while I was awake, so they could be very careful to not cause any problems. And my last surgery with Dr. Berger in 2014, he used a special dye during surgery to highlight the cancer cells, making it much easier to “see” and remove the cancer cells. And with each surgery, he took the effort to not only remove the “seen” tumor, but also buffer around the tumor hoping to remove any “unseen” cancer cells also. Again, art work!
With my 4th recurrence, the GBM was not located “in” my brain but in my dura (tissue) that covers the brain, so Dr, Berger referred me to Dr. McDermott at UCSF that specializes in that! Again, after surgery, I left UCSF having been given amazing care, and leaving with a smile on my face. You can’t find that kind of neurosurgeon here in Southern Oregon. I know there are some web pages that map out the best brain tumor hospitals in the USA. So I highly recommend when it comes to surgery, I’d suggest going out of your way if needed, to find one of the GREAT neurosurgeons, neuro oncologist and radiologists.
If you are hesitant to make the trip to one of the best brain tumor hospitals, I’d at least get referred to them for a 2nd opinion on surgery, chemo and radiation. I’ve known of many people who were told at their local hospital that the tumor was inoperable. Then got a second opinion from places like UCSF, MD Anderson, Duke University, only to be told the tumor could easily be removed! I’d at least get a 2nd opinion before moving forward.
The second question I often get about brain surgery is, “how many can a patient go through?” I’ve been through six; five for recurrences. I truly think that one of the reasons why I’ve made it through six recurrences is that when it came back, if it was operable, I had them GET IT OUT with surgery. My personal belief is that if I had just taken a chemo, or went on some clinical trial only, I would not have made it this long. That’s my 2 cents. Actually research and statistics show that to be true with treating brain tumors.
The next issue that I think is important is getting genetic tests taken from the removed tumor tissue. Each surgery I’ve had genetic tests like EGFR, IDH1, P53, MIB-1, S-100, GFAP, PTEN2, PTEN3, MGMT, OLIG2, NFP, and probably more that I don’t even know about. The important of getting the genetic tests done, is that it helps the oncologist determine which treatments may or may not work well for your personal brain tumor.
Since I was diagnosed in in June 2000 I have gone through radiation twice; first the standard 6 weeks of radiation after I was diagnosed with my first surgery, then again in 2015 the Gamma Knife for my 6th recurrence. I never regret taking both. Yes there can be some long term risks from the radiation, but so far it has not been too damaging. Just recently diagnosed with a mild skin cancer on my scalp where the radiation targeted by left temporal lobe. Also, recently my pituitary has doubled in size, which could be from radiation damage, but unclear for now (going in for a biopsy to see what it is). Again, since I’ve lived 16 years with the GBM, I don’t regret having the radiation.
I’m no pro in trying to describe how radiation works, but here is a simple summary that I got from my neuro-oncologist many years ago. But I’ll start with the very great news is; that over the 16 years since I was diagnosed, the radiation has become way better now than what I got! And now people take the chemo Temodar at the same time they go through the radiation. Temodar was not even FDA approved when I got the radiation, so I had the radiation all alone. So people getting radiation now, are way better off that I had 16 years ago.
Here is my simple understand of how radiation does its job. The radiation only kills your brain cells when they go to divide. Normal healthy cells in your brain only divide about every 5-10 years (for adults). Brain cells are some of the slowest growing / changing cells in our body while we are adults. That is why radiation is much more damaging for children whose brain is still growing and healthy cells dividing all of the time! So, in adults, healthy brain cells rarely divide, but the opposite with cancer cells that divide quickly (at least for most GBMs). That is how the tumor can grow so quickly.
Consequently, the radiation works on killing the cancer cells as they divide to grow. The radiation stays active in your brain over an extended period of time. So even months or years later, if one of your “healthy” or cancer brain cells in the targeted area goes to divide; the cells will die. So there is a chance of long term radiation damage. But again, for me personally, I think it’s worth the risk, when I was fighting a “terminal” GBM brain tumor.
There are different types of radiation. How it aims and hits your brain cells is kind of like the difference between shooting with a “riffle” or a “shot gun”. Gamma / Cyber Knife was more like a rifle. Their aim is very precise and hits very tight on the small area aimed at (the tumor). Where 6 weeks of the conformal radiation, the type many people get when first diagnosed; it is more like a shot gun. It aims at the cancer area and “scatters” that area with radiation. (Sorry if you do not shoot guns, this is probably hard for you to visualize, but gun shooters know what I’m talking about.) So during the 6 weeks of radiation, think of that area of your brain having 100 cells (I know much more!). The radiation scatters over that area, and maybe only 50 of those cells actually get hit. And then it only kills those cells when they go to divide. So often some cancer cells get missed. That’s one reason why we get recurrences.
So during my 6 weeks of radiation, they aim at the tumor area from three angles. My left temporal lobe was targeted, and the radiologists “map” showed it would hit 100% in the smaller area where the tumor used to be. Then from the second angle, it would hit about 70% in the parameter around that area. Then from the third angle, even further away from the tumor, only 30% of that area would get covered. Then the rest of my brain got like only 10% radiated. I hope that helps understand how it targets and works. Again, I’m no doc, but that is how my radiologist simply described it to me (because I always have a million questions for the doctors!)
The Gamma Knife aims differently. It targets and hits a very small precise area. The first radiation took 6 weeks, where the Gamma Knife was a one day event. I was only in the radiation machine for 30 minutes, and I did not “feel” anything at all. I checked into the hospital at 7am and checked out at 1pm. It was pretty fast! The weirdest thing was getting the 4 screws into my skull, to hold my head tight of a metal form, to hold my head VERY still during the radiation. But getting the screws in was not painful.
For me, within 4 months after the Gamma Knife, my MRI showed that all seen GBM brain tumor had shrunk down to nothing seen. Now 1.5 years later, my MRI still does not show any GBM brain tumor.
Unfortunately with both the Gamma Knife radiation and the results of the 6 weeks of radiation people can have necrosis, inflammation, etc. from the effects of the radiation. I did not have any of those problems at all. (But I take many supplements to reduce inflammation and nerve damage from the radiation.) However, each person’s tumor and situations are different, so we all have different results.
When I was first diagnosed in June 2000, Temodar was not FDA approved. The only chemos available were the old type, like BCNU. I was told that it would only add 3 months to my life. So I decided to not take chemo at that time.
Later when I had my first recurrence, Temodar had been FDA approved. I loved hearing that the Temodar felt milder compared to the old chemos. So I decided to take the Temodar. Over my 16 years battling the GBM, I’ve had the Temodar twice; first after my 1st recurrence in 2004, and then again in 2007 after my 2nd recurrence. Each time I took the Temodar, I started it after I had the tumor removed with surgery.
The first time on Temodar I was on it for one and a half years. After that time, I wanted a break and went off on it. But then in 2007 the GBM came back again, so I went on it my second time. That time I stayed on the Temodar for two years. Unfortunately, after that time the Temodar the GBM came back in 2009 while I was still on the Temodar.
That sad thing was, when I had surgery for my 2nd recurrence, the pathology MGMT test showed that my GBM was the type that the Temodar may not even work for at all. I always wonder it taking the Temodar was even worth it. Who knows, but I never regret taking it.
Overall, the Temodar was pretty mild for me. I still had energy enough and felt health enough that while I was on it, I ran in many 5K races, did some mini-triathlons, and did some Mt bike races, and even a x-country ski race, and overall I did good! The more I moved the better I felt. The Temodar did make me feel fatigued during the 5 days each month I was on it, but my energy came back pretty quickly each month when I had the 3 weeks break from it.
Since my Temodar days, I have had 4 more recurrences. Three of which I went back into surgery to have the tumor removed. My 6th recurrence, the tumor was inoperable, so I took the Gamma Knife. During those times, I always reviewed any chemo that may be available, but each time, there was really nothing to choose from, other than again, old chemos that have been out for years. I also looked into clinical trials that were covering news chemos with research, but most of the times I never qualified to be on the clinical trials because I had been through too many recurrence or past treatments. So I have never taken any other chemo, other than the Temodar. Since 2009 when the GBM grew while I was on the Temodar, I have not taken any chemo. So, from 2009 to Feb 2017 I have been chemo free. That is not to say I will not try some other chemo in the future.
During the 3+ years I was on the Temodar, I learned some tips that helped to reduce bad effect I did have while on it. I hope they also help others while on the Temodar.
Constipation: I tried many things in hopes to help constipation. The ONLY thing that seriously helped me was taking magnesium (only in the Ionic Magnesium Citrate form works for me). I take: Natural Calm, a relaxing magnesium supplement by Peter Gillham’s Natural Vitality. It is a powder you put in a cup then add hot water. It bubbles then settles down. Drink it and it tastes kind of lemon like. It works VERY well in softening #2 and keeps you regular. And it does help calm you too!
Heartburn: I had heartburn SO bad. I ended up going to the doc about it. The thing that seemed to help me best was Prilosec. But also making sure I did not eat big meals, but small amounts through the day. Also I made sure I did not eat in the evening after dinner. The later I ate the worse it got sleeping at night. I also got a special pillow that was a “wedge” that got me sleeping in an upward position. So the heartburn bile would not burn my throat. I would definitely try to get the heartburn under control. I had it bad enough that I think it caused damage in my throat, and now I have been diagnosed with “sleep apnea” because I can’t breathe well at night. I think it was caused by the GIRD and heartburn damaging my throat.
Stomach hurting and not digesting well:
Often my stomach felt uncomfortable and hurt some. It was like my digestion was not working well at all. We naturally need enzymes to help digest protein, carbohydrates, and fats. Our whole system gets messed up while on chemo. I began taking Mega-Zyme by Enzymatic Therapy (Protease, Amylase, Lipase) and it help so much. My stomach did not hurt, no gas, no grumbling of my tummy! To digest well, our body also needs the Pro-Biotics. I’ve taken many different brands over time. Recently I have been taking PB8 by Nutrition Now, 14 Billion CFUs a day. Helps so much!
Dehydration: If you get dehydrated at all any negative effects from the Temodar gets worse! Mostly nausea. So make sure you drink lots of water during the day! I put a large pitcher of water on my kitchen counter and made sure I drank a lot of it throughout the day.
Alcohol: Out of the 3 years I was on Temodar, one night, and only one night I got VERY VERY sick and threw up all night. I think because I drank 3 glasses of wine two nights before I took the Temodar. Alcohol can dehydrate you big-time. And you pay the consequences!!! So after that I never drank again!
Temodar Timing: I took the Temodar right before I went to sleep at night. I sat in bed, took the pills, turned the light off, and sleep it off! Don’t take it in the morning like some people do! Why be awake during the worst of it!
Nausea: You should not be feeling nauseous! If you do, you’re not on a good anti-nausea med. One of the best is Kytril. If you feel sick, ask the doc to try a different anti-nausea med until you find one that works for you!
Eating Dinner: Eat a smaller early dinner (like no later than 6:00pm) then eat nothing after dinner. No late night snacks! Eat smaller meals through the day. If I ate too big of a meal, it made me feel worse.
Fatigue and weakness: If on the 5 / 23 Temodar schedule, you get more fatigued and weak the week after your 5 days on Temodar. It is that week your red blood cell count hits its lowest. To boost my red blood counts, I needed some protein with iron, so I ate a big deer/elk/beef steak the week after Temodar. It helped me feel so much better!
Also I took (still do!) Max-Carnitine by Douglas Laboratories (500mg of L-Carnitine) each morning. It sure helps give you some energy!
Depression: Depression can sure hit you hard while you are on chemotherapy! I did everything I could to bring JOY and HOPE into my life! Got out and moved, walk, bike, swim, ski, anything to get my blood moving. It sure helps you see the positive in life! I would tell myself “I am on chemo vacation” and would watch a great movie, laugh at a comedy, listen to great music, work on a puzzle, talk with a great friend, anything to have fun. Makes life seem much better! I exercised 5 days a week for about 40 minutes and it made me feel physically and emotionally better!
Take Naps: My two boys were still in elementary school and they had TONS of energy while I was on Temodar (so I needed energy too!). So each day I would take a one hour nap in the afternoon right before they got home from school. I wanted to have the energy to be the mom they needed when they stepped in the door. The combination of exercise in the mornings & naps later in the day helped me feel so good!
Over the 16 years I have only been on one clinical trial, when I was first diagnosed in 2000. It was a radiation clinical trial at UCSF in San Francisco Ca. It was called H-boc, where they injected me with cow hemoglobin and gave me high oxygen right before the radiation hypothetically to reduce hypoxia and increase the radiation ability. Two weeks in to the clinical trial I had an allergic reaction to the H-boc – so kicked out and had to finish the regular conformal radiation at home in Medford, Or.
Since then I have looked at many clinical trials, hoping to fit into one when I had my six recurrences. However, either I did not qualify due to my recurrences, past treatments, or the genes of my tumor. Also the location of the clinical trial played a roll. Since I live in Oregon, I mostly looked at clinical trials at OHSU, UCSF, UCLA, and a few more that were not too far from where I live in Oregon (well I did look at many in Duke University). I really wanted to be in the vaccine clinical trial they had, and was willing to be at Duke University, but I did not qualify because my tumor was too small in size.
So I was very open to looking at clinical trials, but I also limited myself to ones that were in stage 2 or 3. I wanted to see the results through stage 1 before considering being in it. That may be different in the future if I am desperate, hoping to survive, and have no other choices.
Overall, I am very thankful for the research and clinical trials out there! They are one of the things that gives me hope for the future, not only for myself, but for all of us brain tumor fighters that hope for a cure.
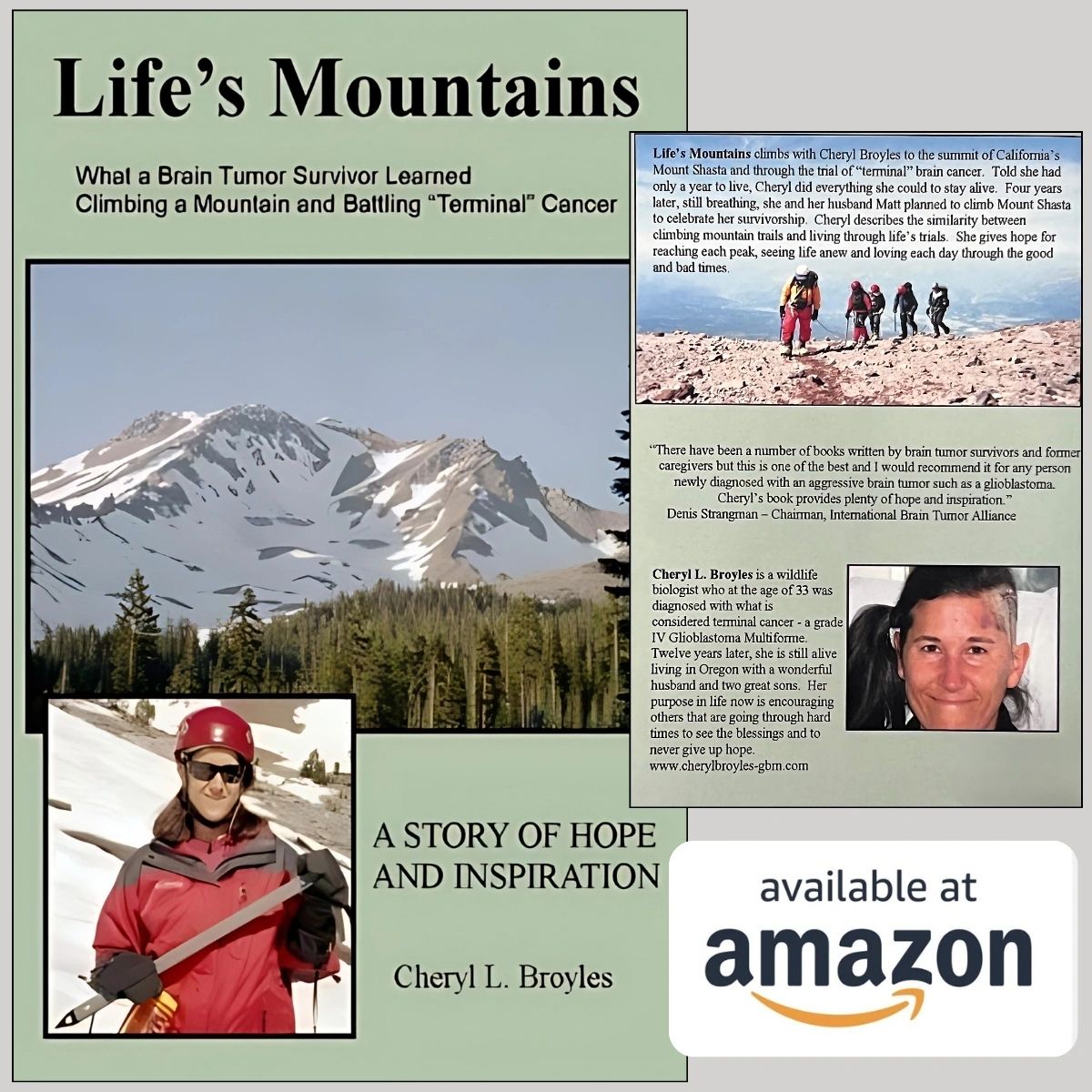
Learn more about my journey from my inspirational book!
Life's Mountains: What A Brain Tumor Survivor Learned
Life’s Mountains climbs with Cheryl Broyles to the summit of California’s Mount Shasta and through the trial of “terminal” brain cancer. Told she had only a year to live, Cheryl did everything she could to stay alive.
Copyright © 2024 Cheryl Broyles - All Rights Reserved.
Powered by GoDaddy
This website uses cookies.
We use cookies to analyze website traffic and optimize your website experience. By accepting our use of cookies, your data will be aggregated with all other user data.